HPA Axis Dysfunction: Ways To Destress & Heal Your Adrenals
The stress response isn’t just one gland; it’s more of a complex symphony involving the hypothalamic-pituitary-adrenal axis (hence the name “HPA axis” dysfunction).
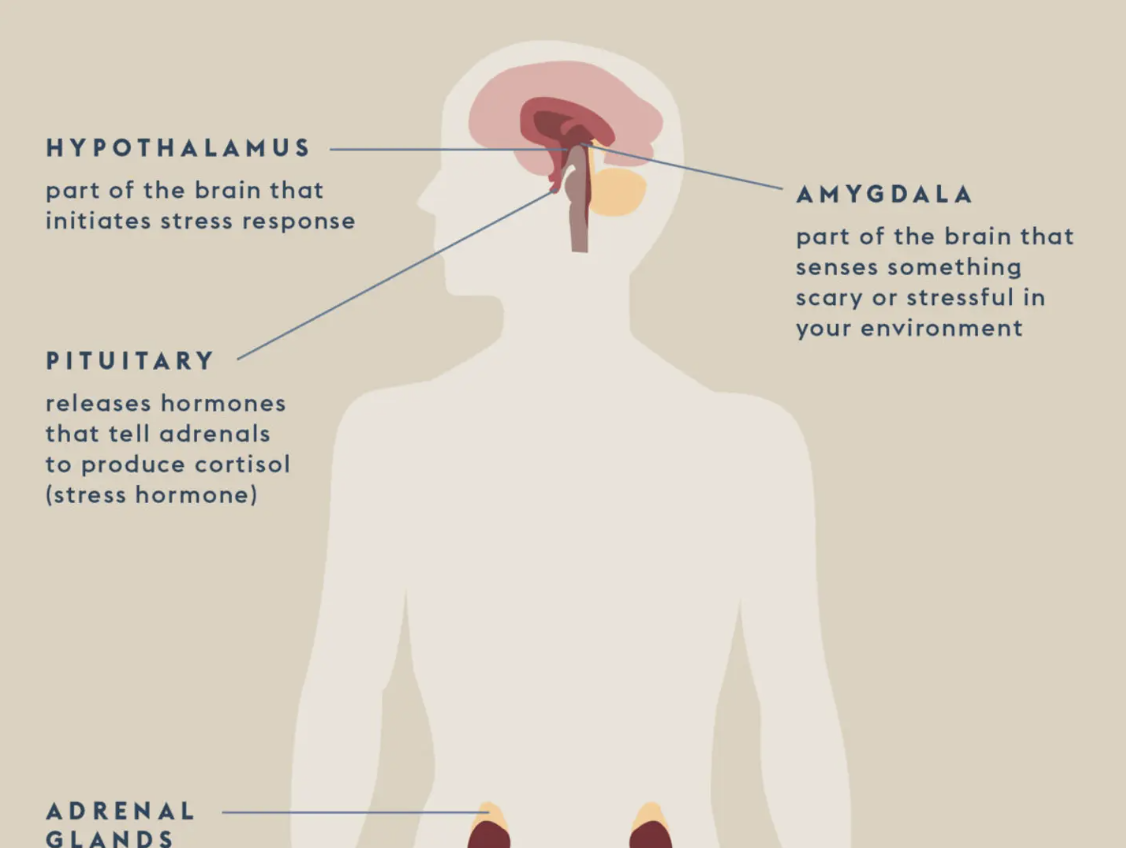
Image by Parsley Health
This symphony involves the adrenal glands, yes, but also the amygdala (the part of the brain that senses something scary or stressful in your environment), the hypothalamus (the part of the brain that initiates the stress response), and the pituitary gland, which receives messages from the hypothalamus and releases hormones that tell the adrenals to produce cortisol, among other things. With HPA axis dysfunction, constant activation of this symphony causes the communication between the hypothalamus and the pituitary and adrenal glands to go haywire, which leads to unhealthy changes in the way the body produces cortisol and other hormones and neurotransmitters related to the HPA axis, such as melatonin and epinephrine.
As Dr. Gonzalez explains, “It’s an entire cascade of events that are happening way above the level of the adrenal glands.” When we focus on just the adrenals, we’re missing the full picture. “The term adrenal fatigue is a myth,” she says.
Your adrenals are a part of the HPA axis (hypothalamic-pituitary-adrenal) and secrete various hormones, including cortisol.
When we face a stressor, our hypothalamus releases corticotropin-releasing hormone (CRH), which triggers the release of adrenocorticotropic hormone (ACTH) from the pituitary gland; ACTH then travels through the bloodstream to the adrenal glands, where it triggers the release of cortisol, a steroid hormone.
Cortisol is the hormone that prepares our body for the “fight or flight” response when we perceive a stressor.
Our HPA axis works on a feedback loop which means that when the hypothalamus and pituitary gland receive signals that high levels of cortisol have been released from the adrenals, they put the breaks on CRH and ACTH to stop triggering more cortisol release.
But in cases of chronic stress, it can cause a dysfunction in this feedback loop. The HPA axis can become desensitized over time and will not properly respond to stress signals. When this occurs, we get the common mislabel of “adrenal fatigue.” But your adrenals are NOT fatigued. This is all just a part of a complex feedback loop mechanism that has become desensitized over time.
What causes HPA axis dysfunction?
First, it’s important to remember that stress isn’t an inherently bad thing. In fact, as Dr. Gonzalez points out: “We wouldn’t survive without it.” With that said, the stress response is meant to work acutely in dangerous situations. Chronic stress does a lot to you metabolically; it causes sugar cravings, shuts down digestion, and affects your sleep!
What Triggers Dysfunction in the HPA Axis? The HPA axis dysfunction is influenced by two primary forms of stress: immediate (acute) stress and chronic stress. Prolonged exposure to chronic stress can impede the optimal functioning of the HPA axis, necessitating lifestyle and dietary interventions for restoration. Identifying the various cumulative stressors that contribute to HPA Axis dysfunction is crucial. These stressors encompass a broad range, including:
Stress: Stress, in its diverse forms, serves as a comprehensive term covering internal and external influences that induce malfunction. Mental, emotional, physical, chemical, and biochemical stress all fall under this umbrella. Lifestyle stressors, such as insufficient sleep, disruptions to the circadian cycle, and emotional stress (e.g., financial strain, recent breakup, relocation, or major life changes like death), are part of the stress spectrum impacting HPA axis functioning. Undiagnosed infections, exposure to environmental toxins (like mold, pollutants, pesticides, and endocrine-disrupting plastics), and dysregulation of the inflammatory response can also adversely affect the HPA axis.
Inflammation: Maladaptive inflammatory responses can lead to HPA axis alterations. Excessive activation of the HPA axis due to inappropriate stress responses has been linked to increased inflammation. This unchecked stress response can subsequently trigger an inflammatory reaction. Inflammatory factors stimulate the HPA axis to produce more cortisol, and prolonged inflammation can foster chronic HPA axis activation. Elevated cortisol levels, in turn, contribute to an inflammatory response in the body, disrupting the normal function of the HPA axis pathway in the brain, which controls other hormones in the body.
Nutrition: The body's demand for nutrients increases during periods of stress. Key nutrients that may become depleted during HPA dysregulation include B vitamins, Magnesium, Vitamin C, and Zinc, as well as digestive enzymes and HCL. It is advisable to avoid processed, refined, and high-sugar foods that can have negative effects on the HPA axis. Maintaining a balanced and nutrient-rich diet becomes essential to support HPA axis function during stressful periods.
How Does HPA Axis Dysfunction Affect Our Health and Wellbeing?
As time passes, our nervous systems undergo a gradual strain, becoming overloaded and overstimulated. This prolonged stress can lead to the dysregulation of the stress response. Consequently, there's a risk of overactivating the HPA axis, triggering the activation of diverse inflammatory pathways. This overactivation can have adverse effects on mood, hormones, fertility, immune function, energy levels, and metabolic function.
HPA axis dysfunction symptoms
Research has shown a link between HPA axis dysfunction and impaired cognitive function, inflammatory and autoimmune diseases, mood disorders, and more. “Chronic stress and HPA axis dysfunction affect every major organ system in the body,” says Dr. Gonzalez. Knowing this, it shouldn’t be surprising to learn that the symptoms of HPA axis dysfunction are life-disrupting, vague, and widespread. Here are some of the important ones to look out for:
Feeling chronically exhausted and fatigued
Feeling tired but wired
Unexplained weight gain or weight loss (weight gain may be seen around the hips and belly area)
Poor quality sleep (which can include waking up feeling unrefreshed even after getting hours of sleep)
Trouble falling asleep or staying asleep
Poor immune response
Brain fog, difficulty concentrating, and poor mood (including anxiety and depression)
Increased cravings for sugar and salt
Poor circulation, inflammation, and feeling "puffy"
Hair loss and weak nails
Hormone imbalances such as changes to the menstrual cycle (shorter or longer cycles, as well as completely missed periods)
How to heal from HPA axis dysfunction
While it’s important to address major sources of stress, like toxic people and workplaces, if you have HPA axis dysfunction, getting back on your feet does not mean avoiding stress altogether. “We’re not going to get rid of stress anytime soon, so we need to create more tolerance to it,” says Dr. Gonzalez.
A good place to start is identifying what’s most important in your life. See your energy as a bank account of commitments and try to scale back.” This is also a good time to go back to the basics, focusing on improving sleep hygiene, eating a healthy diet, and trying meditation. Your body wants to heal, so try not to get in the way,
According to Dr. Gonzalez, caffeine also has a role to play here. “Coffee is often used as a form of self-medication to deal with fatigue,” she says. Still, caffeine can heighten the sense of alarm the body experiences and increase the release of catecholamines, the hormones secreted by your adrenal glands. As Dr. Gonzalez points out, “It’s not sustainable and can perpetuate the problem.”
Functional Medicine Treatment for HPA Axis Dysfunction
Nervines and adaptogens emerge as highly effective treatments in functional medicine for supporting the HPA axis.
Adaptogens, characterized by their innocuous nature, play a non-specific role in enhancing resistance against various stressors—be they physical, chemical, biological, or psychological. This unique class of healing plants, including Eleuthero, Rhodiola, Cordyceps, Ashwagandha, Schisandra, and Tulsi (Holy Basil), contributes to balancing, restoring, and protecting the body. Incorporating these adaptogens into long-term strategies proves beneficial for maintaining the health of the HPA axis.
On the other hand, the term nervine encompasses a diverse range. Broadly defined, nervines are plants or herbs that positively influence the nervous system. They come in stimulating, calming, and intermediate varieties, primarily working to support relaxation, manage stress, and promote overall nervous system well-being. Notable nervines such as Kava, Albizia, Passionflower, Milky Oats, and Skullcap offer support for addressing HPA axis dysfunction.
Try to focus on balancing blood glucose levels by getting enough quality fat, protein, and fiber. Be sure to increase your intake of folate, magnesium, and sulfur-rich veggies, such as broccoli, Brussels sprouts, kale, spinach, and cauliflower. Also, increasing your intake of Vitamin D, which acts as a pro-regulatory hormone in the body, can reduce inflammation and support immune cell production
You should also prioritize sleep, ideally getting to bed before 10:00 PM and aiming for 7-9 hours of sleep per night. Acupuncture, low-intensity exercise, and even nature therapy (such as grounding or forest therapy) can all effectively support the HPA axis.
More Actions You Can Take Today To Help Heal Your Adrenals
Try finding time to integrate more self-care practices such as Epsom salt baths, deep breathing exercises, yoga, massage, walking outside, meditation, journaling, and anything else that brings comfort and builds stress resiliency using vagus nerve toning exercises like diaphragmatic breathing.
Practice meditation: Spend five minutes on an app like Headspace, Calm, or Insight Timer for short guided meditations. Meditating can take many forms and does not have to be long and drawn out.
The most important thing is not to skip meals, always eat breakfast, and avoid going more than 4 hours between meals or high-quality snacks.
Avoid staying up late past 10 pm as much as possible (more restful sleep happens before midnight).
Consume Adaptogen Blends- Adaptogenic herbs have been shown to positively affect stress reduction, adrenal function, and thyroid function. Adaptogens have also recently been researched for their anti-cancer, hepatoprotective, and immunomodulatory properties. Click HERE for great articles on the role of adaptogens. Adaptogens that are great for stress: Ashwagandha, L-theanine, Eleuthero root extract, Licorice root, Rhodiola, Holy Basil, and. Schisandra
Support your adrenals and gut by decreasing caffeine consumption; instead, try green tea, matcha, or no caffeine options: Dandy Blend (dandelion root tea), herbal tea, herbal chai, and decaf coffee. Org Coffee brands/ alternatives: Four Sigmatic, Lifeboost. Rasa, Four Sigmatic Chai Latte, or MUDWTR.
Move your body daily - Getting outside in the fresh air affects your pineal gland and helps reset your brain and the stress response. I recommend low-impact workouts like walking, pilates, yoga, barre, etc.
Try regular rhythm. Rhythm is key because your hormones are balanced in rhythms. So, waking up at the same time every day, going to bed at the same time every day, and eating at the same time every day help reset your natural balance.
Add essential vitamins and minerals that support adrenal gland function, immune system function, and stress hormone metabolism. Vitamin A, vitamin C, and zinc play a role in healthy immune system function, while Pantothenic acid (vitamin B5) is a cofactor for cortisol production.
Written & edited by: Dr. Gonzalez, & Cameron Gildea, INHC.The information and supplements provided is not medical advice and is not intended to treat, diagnose, cure, or prevent any disease. Always consult your doctor before starting any new supplement or health routine.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5666903/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4688585/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860380/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3166406/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4045534/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3991026/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4790408/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7352613/
https://www.rupahealth.com/live-classes/understanding-the-cortisol-awakening-response
https://www.rupahealth.com/post/wired-but-tired-this-isnt-a-normal-part-of-aging